CALCIFICATION ON THUMB BASE ( OSTHEOARTHRITIS OF CMC JOINT OF THE THUMB)
1. CALCIFICATION ON THUMB BASE
(Osteoarthritis of the Thumb Basal Joint)
The thumb allows very special movements in a harmony with the other fingers. Most of these movements particularly pinching and gripping are possible with a functional basal joint (carpometacarpal joint) of the thumb. Because of its unique design it tends to develop earlier arthritis than those in the fingers. Destortion of this joint results in pain when it moves. Arthritis of thumb basal joint is seen more in women, older than 4o years of age.
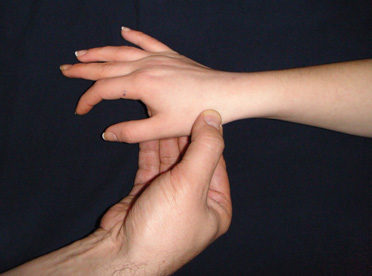
During physical examination, pain and loss of power whilst pinching or gripping, swelling and/or tenderness at the base of the thumb(picture 1), limitations in joint movements are noticed. Patient and doctor may feel friction if the thumb is tried to move in different directions when proksimal part is keeping stabil.
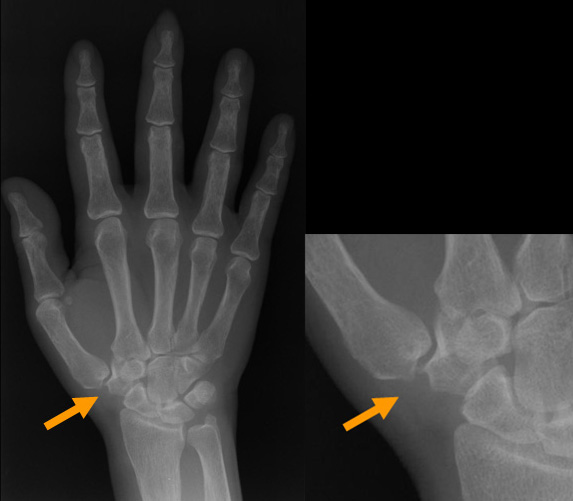
X Ray reveals distortion in congruence(dislocation) and cartilage surfaces of the joint, bony spurs(picture 2).
In the early stages, positive response could be obtained with non-surgical methods. Ice application several times a day, 5-15 minutes each time, aspirin or non-steroid antiinflammatory drugs may be helpful for pain and swelling relief. Supporting splints limit the joint movements and helps lessening the pain(picture 3). Steroid injections may be also helpful for pain relief.

If conservative methods fail, arthroscope assisted closed surgical approach is next treatment of choice(picture 4). The joint can be visualized directly by an arthroscopic camera. Very fine(1.9-2.4 mm diameter), high technology cameras and instruments are used for this surgery. Bony spurs can be shaved and hypertrophied synovia can be removed. Dislocation of the joint is corrected using a tight rope. Using this rope, first metacarpal is brought to its proper anatomical position with the carpal bone trapezium(picture 5). After surgery, no splint needs to be worn, and patient is allowed to use his or her hand as soon as possible. So, these patients can return to their work earlier.One of the main advantage of this surgery is to keep the commonly preferred methods as described below for the failed and severe cases.
For end stage cases (severe degenerations on the joint and bone surfaces) or elder patients whose bone dansity is poor, to remove the damaged parts or trapezium(carpal bone)is the solution. Some tendons are used for suspension of the thumb and to fill the empty space after bone removal. After this surgery, plaster splints are worn for several weeks. This surgery also works very well for pain relief. It only affects the grip power after surgery compared with the camera assisted method.
-

(picture 4)
-

(picture 5)








